Q&A: Rights vs. Policy, Cervical Checks, and Bishop Score
In this episode of the Breath and Birth Co. podcast, Vanessa, a Certified Birth Doula and Childbirth Educator, addresses key questions about labor and birth. Vanessa explores essential topics including informed consent, the information gained during a cervical check, and what constitutes a Bishop score. She explains your rights throughout the birthing process, stressing the significance of bodily autonomy and informed decision-making. Additionally, Vanessa provides insights into the three crucial measurements taken during a cervical check—dilation, effacement, and station—and which piece of those measurements can impact the progression of labor most. The episode concludes with a detailed look at the Bishop score and how it can predict the likelihood of a successful induction. Vanessa also highlights the value of comprehensive childbirth education and discusses her online course, 'Metamorphosis'.
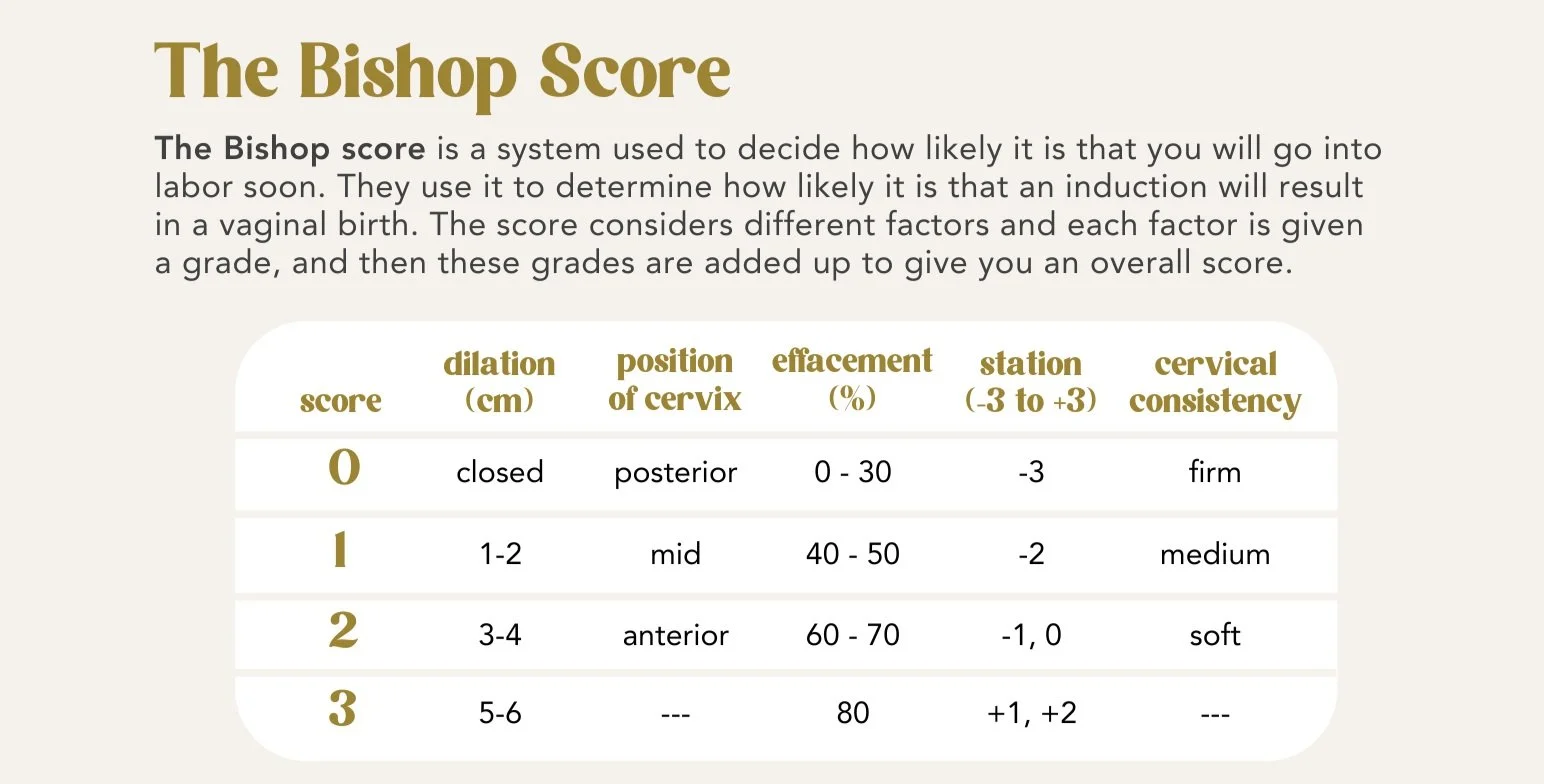
This Bishop Score matrix is an excerpt from the “Guide to Induction,” offered as part of the “Inductions & Augmentations” lesson in the Confidence module of Metamorphosis.
-
-
00:00 Welcome to the Breath and Birth Co. Podcast
00:47 Introduction to Today's Q&A Session
01:02 Understanding Your Rights in Labor and Birth
01:51 Informed Consent and the BRAINS Acronym
05:02 Navigating Hospital Policies and Your Rights
05:55 Cervical Checks: What They Mean and Your Rights
09:28 The Importance of Baby's Station During Labor
12:30 Understanding the Bishop Score
15:07 Childbirth Education and Resources
17:21 Conclusion and Final Thoughts
-
Vanessa: Welcome to the Breath and Birth Co. podcast. I'm Vanessa, a hospital based, DONA- International certified birth doula, and passionate childbirth educator. I love to merge the power of your intuition with the precision of modern medicine to help you navigate pregnancy and birth your way. Each week we kick off with Monday meditations to bring calm and connection to your pregnancy.
Then we build your confidence through insights, birth stories, and care provider perspectives during thoughtful Thursdays. Ready to feel supported, informed, and empowered? Hit subscribe to the Breath and Birth Co. podcast today and let's embark on this transformational journey together. As a reminder, any information shared here is not medical advice.
For more details, visit breathandbirthco. com slash disclaimer.
Okay, so today's episode, we're going to dive into a Q& A session with three separate questions. Um, but I'm pairing these together because they're all somewhat related, and so I thought that would be a good way to cover all of these bases. So first, , I'll start out with what are my rights in labor and birth?
And this is an excellent question and really my answer applies to anything medically related in any period of your life. But I'm pulling answers here from the what's allowed in my legal rights lesson in my Confidence module of metamorphosis.
So yeah, so first, let's break down your rights. You have the right to information about interventions. You have the right to refuse any medical test or procedure, and that includes during pregnancy, not just labor and birth. And you also have the general right to bodily autonomy. So anything that is happening to your body, you have the right to say yes or no to.
, which leads me to informed consent, , informed consent is your legal right and it's described as the willing acceptance of a medical intervention by a patient after adequate disclosure by the physician. Disclosure of the nature of the intervention with its risks. And alternatives there's also a guide that comes with that lesson in metamorphosis that goes more in depth into ACOG, which ACOG stands for American College of Obstetricians and Gynecologists, and it's the organization which establishes clinical guidelines and resources for women's health care providers that are evidence based.
So it's,
It's kind of the gold standard that they should be following based on evidence. , and anyway, so the guide in my lesson does go over ACOG's actual recommendations. And it covers ACOG's position on informed consent, the essential elements of informed consent process, which include diagnosis, nature and purpose of the recommended interventions, alternative treatments and options, as well as the risks and benefits of all options, including foregoing treatment altogether.
And then it also covers the shared decision making piece of it. , I do want to say informed consent is not signing a consent form upon entering the hospital. You will be required to sign some paperwork upon admission and that is not informed consent. Informed consent is having the opportunity essentially to run through the BRAINS acronym with your provider at any crossroads or during any discussion.
Um, and I honestly can't remember if I've covered BRAINS at all in any of the podcasts we've recorded so far. So I'll go ahead and run through that right now for you too, even if it's just a refresher. So BRAINS is an acronym where B stands for Benefits, R is for Risks, A is Alternatives, I is Intuition. N is nothing or not now.
And S is space. So B is benefits. What are the benefits of what you're proposing right now, whether that's an intervention or a test or procedure? What are the risks of this, , intervention or procedure? Are there alternatives? What's my intuition telling me right now? N is for nothing or just not now. An S is for space and that is space to process the information that you've just been given to be able to give a fully informed consent and have time to process and have all of the feelings, and the opportunity to ask more questions if needed.
Being able to run through BRAINS and getting all of the answers that you need is an example of being able to give informed consent or declining.
So, keep in mind that while hospital policies are written to provide a safe environment and quality care to patients, they're also written to prevent liability.
And so, in terms of what's your right versus what's, what's allowed or what's hospital policy, just keep in mind that hospital policies are ultimately written to prevent risk of lawsuit for a business entity that exists to . make a profit. , so just remember that perspective, too. If any of your providers happen to throw out well, policy says this, or I can't, you're not allowed to do that because hospital policy says this.
That is not your right, , to bodily autonomy and making an informed decision for your body and your baby. So just remember that
Okay, so I think that covers that Let's move on to question number two, which is what are the numbers during a cervical check and what do they mean? So first, tying back to the informed consent piece, cervical checks are not medically necessary and you should give informed consent every time if you choose to have one.
And you do have the right to refuse a cervical check and they will likely or often offer you a cervical check as if they are just going to do it. Like, for instance, a nurse might come into the room, either during a prenatal appointment, or while you're actively in labor, and say, okay, you are X amount of weeks along now, or it's been X amount of hours since we've last offered a cervical check.
I'm going to go ahead and check you now. That's not informed consent and it's also not necessary and you have the right to say no Thank you. Not now or I'd like to wait a little bit or I'm not interested in cervical checks at all And you also have the right during a cervical check if you do initially consent to it If it's painful, you're uncomfortable in any way if it's you know, inducing trauma in you.
If you say stop, it is your provider's role to stop and immediately remove their hand. , and if they do not, that's a form of obstetrical violence, , and it should be addressed accordingly.
Okay, so if you do choose to have a cervical check, you'll likely be given at least one measurement. Um, typically that's the dilation, but technically your provider should inform you of three different measurements. And each of these can be important in determining, um, where you're at in labor.
It's not going to be a magic or a crystal ball and telling you how long labor will last or when your baby will arrive. These are just snapshots in time. Labor is not linear. , but these three measurements. Each tell you something different. So there is dilation, which is how open the cervix is, and is measured 0 to 10 centimeters, where 10 is often referred to as being fully dilated or complete.
Then there is effacement, which is how thin the cervix is. And that's a measurement that's given in a percentage from 0 to 100%, 100 percent being fully effaced. And then the third number is a station. And this is where baby is in relationship to the pelvis, measured from anywhere from negative 3, negative 5, all the way to plus 3 or plus 5, depending on who you ask.
, so those can vary, but generally speaking, it's from a negative number, Zero being, the mid pelvis, and then the positive number. That negative three is the pelvic inlet, which is higher up in the pelvis, so baby's not totally fully engaged yet. Zero, again, is going to be at that mid pelvis station, and plus three is at the pelvic outlet, very, very low.
, plus three is basically crowning. , and all of this information is broken down into more detail in the understanding baby's position lesson in my foundation module of metamorphosis. Um, but given all of that information, as a birth doula, baby's station actually tells me more than dilation.
It's telling me which positions are optimal for me to encourage you to try. , for instance, do we need to create more space in the pelvic inlet or the outlet? Certain positions, in the way that your body or your legs are oriented, can open the inlet or the outlet. So I want to make sure that I know where baby is so that I'm not doing the opposite of what we want.
We want to create space for baby wherever they're at to further descend into and through the birth canal. And then also, if you are consenting to consecutive cervical checks every few hours, I'm listening to, if baby's been chilling at the same station for a while, there may be some other, factors too, where baby might be asynclitic or in a wonky position, and so that can help with determining.
Also positions to put your body in, um, perhaps we need to try a Spinning Babies (R) routine, um, and I'll link details about that in the show notes as well. Um, but yeah, once baby descends, their head will put pressure on the cervix and help dilate and efface that cervix more. So ultimately, the goal is to get baby down and into and through that pelvic outlet.
So that's why station, Actually means more to me than dilation. But often times when you're checked, the nurse or the provider will just say, Oh, you're 4 centimeters, or Oh, you're 6 centimeters. And then that's it. End of conversation. So make sure that you, your partner, or if you have a birth dual in the room, really ask for all three of those measurements.
, especially the station. I would rather hear that first. And sometimes they're like, Oh, I didn't really check. So they, you know, they might have to go back in there. So, um, again, just advocating for that while they're checking, maybe prompting the question. Either ahead of time, I'd really, I'm really interested in knowing what station baby's at, or as they're telling you, the measurement, you can say, Oh, are you able to tell me, what station baby's at?
And even some amazing providers and nurses might be able to feel, the skull and be able to tell you what position specifically in terms of right, anterior, posterior, left, etc. Um, that it is, based on the, ridges in the baby's skull. And so, again, they might not be able to tell you that, but some are really good and baby might be in an optimal position for them to be able to do that. , it can also be really painful and you might not want that. So anyway, um, yeah, so those are the three measurements that are typically given during a cervical check.
The third question of today's Q& A episode is, What is a Bishop score and how is it used? And this is a great question and again aligns with the other topics of informed consent and cervical check measurements. So, especially if you've been approached for an induction, you may have heard of the Bishop score. And I do cover this in the "Induction and Augmentation" lesson of the Confidence module for metamorphosis. And have a guide to induction that outlines the Bishop score matrix and how to interpret your individualized score, along with some other things.
And I'll include that matrix in the show notes too for quick reference. Basically, the Bishop score is a system used to decide how likely it is that you will go into labor soon, and how likely it is that an induction will result in a vaginal birth. So this score considers different factors, and each factor is given a grade or assigned a number, and then those numbers are added up to give you an overall score called the Bishop score.
Each factor's, uh, rated on a scale of zero to three. Some of them only go to two, but, you'll notice that in the matrix. And then the factors include dilation, which we just talked about, position of cervix, which is posterior, mid, or anterior, then effacement, which again we just talked about, station, and the fifth factor is cervical consistency, which is measured as firm, medium, or soft.
So again, each of those individual factors is rated on a scale of 0 to 2 or 0 to 3, depending on the factor. And then you're going to add up each of those factor scores to get your total Bishop score.
If your score is high, it means there's a better chance that an induction will lead to an established labor pattern.
For instance, if your score is 8 or higher, it's a good indication that spontaneous labor might start soon. If your score is five or below, that's an example that might mean your labor is much less likely to spontaneously start soon and an induction is unlikely to be successful yet. Um, so yeah, so take that information for what you will.
And again, all of this information is in, my online self paced metamorphosis childbirth education course, which I'll link in the show notes as well.
If you're pregnant for the first time and or asking yourself any of these questions, I highly recommend seeking out a childbirth education course. While your local hospital probably offers courses, I'm going to be honest, they tend to teach you how to be a good patient. Those hosted outside of the hospital setting tend to be much more comprehensive And hopefully you'll be able to find a specific method or teacher that you truly resonate with.
I offer an online self paced course called Metamorphosis, so I'll plug that one now. Metamorphosis is a transformational, self paced, comprehensive online childbirth education course. It's almost 8 hours of video content spread across 50 lessons. in four modules and comes with over 200 pages of guides and worksheets and affirmations at every step.
In the foundation module, you'll determine your why and learn what a physiological birth looks and feels like and how baby station can mean more than your cervical dilation.
In the Connection module, you'll ensure your care provider is aligned with the birth you envision, and how to build out your village in a way that sets you up for best success all the way through postpartum.
Then, there's the Confidence module, where you'll learn all of your options and be equipped with evidence based resources to make an informed decision each step of the way, culminating in your very own birth priorities plan.
And last, but certainly not least, in the calm module, you'll release fears that are holding you back from the birth you envision and infuse peaceful meditations into your daily routine. Then practice proven pain coping methods to prepare you for labor.
Knowledge is power, and I'm so grateful that you're here listening to this episode. And if you're interested in childbirth education, but self paced online learning is not your cup of tea, or you may have a specific method that you're looking for, there's no gatekeeping here.
In that case, I have a referrals page on my site I'll link in the show notes for various other Columbus, Ohio, local and live online options in case any of those would be a better fit for you. Again, I just want to encourage and empower you to have the information you need to advocate for the birth you desire.
Thank you so much for spending time with me today. I hope you found this episode helpful and encouraging on your journey. Don't forget to hit subscribe so you never miss a future episode. And if you enjoyed today's conversation, I'd be so grateful if you left a quick review. It helps others find the show.
For more information, Resources and links mentioned in this episode. Be sure to check out the show notes. You can also connect with me on Instagram at breath and birth. co for more support and inspiration until next time, remember you've got this and you're never alone in this journey.